Social Drivers of Health (SDOH) are the conditions in the environments in which people live, including where people are born, live, learn, work, play, worship, and age that affect their health and quality of life. To address the social drivers of health, a health center should seek to universally screen patients for social needs throughout the practice and connect patients to community resources.
It is well documented that social drivers have a significant impact on health outcomes. In the value-based care environment, success is based on health outcomes. Importantly, addressing patients’ health-related social needs can improve quality of care and = patient experience and thus is critical to success in value-based care.
Universal screening and connections to community resources will look different at each health center and will largely be driven by the needs of the population, the resources available in both the health center and the community, and the priorities of the health center.
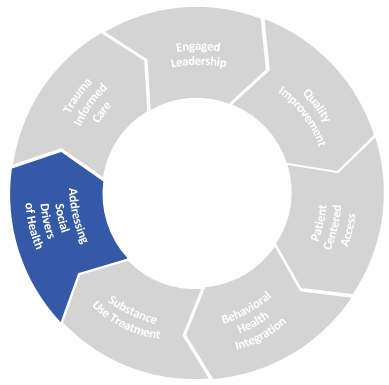
Drivers of Success:
- Workflows, protocols, and the care team to support screening and referrals
- Strategic partnerships and investments in the community
- Technology and tools meet the needs of all partners
Engaged Leadership in Action: Social Drivers of Health
- Leadership team seeks out opportunities for partnerships with community-based social service organizations.
- Leadership team sets the expectation that addressing health-related social needs is a key driver for achieving health equity.
- Leadership team ensures Community Health Workers (CHWs) and other peer-support roles are valued members of team responsible for addressing social drivers of health. CHWs are included in planning conversations around how to address health-related social needs (HRSN) and their expertise in understanding and responding to them is leveraged.
-
Partner Resource
Insights from our partnerships to address social health
Source: Community Care Cooperative
Learn more about how partnerships to address social health bridge the gap for patients
Read blog post -
Partner Resource
C3’s Flexible Services Program
Learn more about the Flexible Services Program model and C3’s approach, hear from our social service partners, and get tips and ideas to advance your members’ and community’s health-related social needs
Visit website -
Partner Resource
C3’s Flexible Services Program: Executive Summary
Source: Community Care Cooperative (C3)
Learn more about the Flexible Services Program model and C3’s approach and impact
PDF ↓
Workflows, Protocols, and the Care Team to Support Screening & Referrals
Getting Started
Screening for health-related social needs, making referrals, and conducting warm hand-offs to social services organizations in the community requires a team-based approach.
For a health center that is new to screening for social needs, the following tips can help the planning team get started:
- Learn about the social services organizations in the community that currently serve the health center’s patient population; leverage the expertise of community health workers and other peer support care team members for this exploration.
- Engage multiple stakeholders, including social service organizations, early in the planning process.
- Assess the current processes and workflows for other screenings (e.g., depression screening, pediatric developmental screening). When possible and practical, align screening for social needs with other screening workflows.
Care Team Considerations
The care team member that screens a patient for social needs may be different than the care team member that responds to the patient’s needs. However, it’s important that protocols are in place to ensure that patients’ unmet social needs (positive screens) are responded to in a timely manner.
Various care team members may play a role in identifying patients’ social needs:
- A receptionist at the front desk may administer a social need screening questionnaire on paper or a tablet for a patient to complete on their own while they are waiting for their appointment.
- A medical assistant may conduct a verbal social needs screening while they are rooming a patient.
- A Community Health Worker may conduct patient outreach and administer a phone-based social needs screening.
- A provider may make a warm handoff to a CHW during a patient’s visit to complete a social needs screening.
- Family partners, care coordinators, and peer support members may play a role in identifying and responding to patients’ health-related social needs.
When identifying a workflow for social needs screening, it’s important to understand the needs of the community and patient population. For example, a health center that serves a large population of patients experiencing homelessness may find it beneficial to include a housing specialist (or a CHW with particular expertise on navigating housing issues) on the care team. Health centers will need to determine how much internal expertise and case management they wish to provide, and determine when they will refer patients to outside community-based SSOs.
Training
Ongoing training for community health workers and other care team members who support patients in this work is incredibly important. Trainings should cover tools and techniques CHWs can use to successfully engage members in conversations about the social circumstances and also build their knowledge base of community resources and strategies to address unmet social needs.
Examples of trainings include:
- How to gain trust with patients and engage in conversation about health-related social needs using motivational interviewing techniques
- How to use trauma-informed approaches to reduce harm, stigma, and judgement
- How to find resources, including trainings on various public benefit programs and community programs
Strategic Partnerships and Investments in the Community
A health center can take various approaches to responding to patients’ health-related social needs:
- Referral: Refer a patient to a social service organization by providing the patient with a phone number to call or an address to visit. While this may be the simplest approach, it is often not a successful strategy for ensuring that patient’s ultimately access the service
- Closed-loop referral: track the referral and follow up with the patient to ensure their need has been met
- Warm Handoff: While the patient is present, connect the patient with the SSO and ensure the SSO has the information they need to support the patient
Building trusting partnerships with community-based social service organizations (SSOs) and engaging those partners in the design and implementation of a health center’s screening and referral process is key. Community-based SSOs have the expertise in responding to patients’ social needs; however, the need for support is often much greater than the resources that are available at these organizations. This can often, unfortunately, result in referrals to an organization that does not have the capacity to take on additional clients. That’s why it’s important to engage these organizations early in planning efforts. Understanding their program requirements and intake processes will help make referrals more successful.
When possible, health center leaders should consider leveraging grants or other funding opportunities to expand capacity at SSOs. Other opportunities to expand capacity at SSOs include supporting opportunities for improved data sharing between health centers and SSOs and convening multiple SSO partners to discuss promising opportunities and strategies for effective partnerships.
-
Resource
Levels of HRSN & SDH Integration Framework
Source: Health Begins
A six level framework to help healthcare and social service partners address health-related social needs. The first level begins with coordination and moves through increasing levels of collaboration and integration.
PDF ↓ -
Resource
Building Strong Community Partnerships to Address Social Needs
Source: CMS
This case study from the Accountable Health Communities Model highlights strategies for engaging community advisors to facilitate cross sector collaborations
PDF ↓
Technology and Tools that Meet the Needs of All Partners
Screening Tools
There are numerous screening tools that can be used to assess health-related social needs at the patient level. Choosing a reliable tool and using it consistently ensures that you accurately track and monitor this important information.
-
Resource
State of Science on Social Screening in Healthcare Settings
Source: SIREN (Social Interventions Research & Evaluation Network, UCSF)
The goal of this report is to synthesize and disseminate recent research on social screening.
PDF ↓
-
Resource
PRAPARE Screening Tool
Source: https://prapare.org/the-prapare-screening-tool/
Protocol for Responding to & Assessing Patients’ Assets, Risks & Experience (PRAPARE) is a national standardized patient risk assessment protocol designed to engage patients in assessing & addressing social drivers of health (SDOH).
Visit website -
Resource
Standardized Screening for Health-Related Social Needs in Clinical Settings: The Accountable Health Communities Screening Tool
Source: National Academy of Medicine
PDF ↓ -
Resource
The Hunger Vital Sign
Source: Children’s HealthWatch
The Hunger Vital Sign is a validated 2-question food insecurity screening tool based on the U.S. Household Food Security Survey Module to identify households at risk of food insecurity.
Visit website
Referral Platforms
Many health centers may currently maintain a list of community resources with phone numbers and other contact information. It can be time consuming to maintain these lists and keep the content up to date. There are numerous platforms and tools that can provide support by maintaining resource databases.
In addition, some platforms and tools provide mechanisms for making and monitoring referrals. It’s important to accurately monitor and track this data for many reasons:
- Understanding the breadth of needs at your health center can help determine where to focus your efforts and recourses
- Data on referrals can be useful for your partner SSOs. it can help them understand the demand for their services and help them advocate for more funding and resources
- Sharing HRSN data between health centers and SSOs helps partners to investigate the drivers of HRSNs and direct resources towards addressing those upstream challenges
-
Resource
Adopting a Community Resource and Referral Platform: Considerations for Texas Medicaid Stakeholders
Source: Center for Health Care Strategies
This brief shares experiences from Medicaid stakeholders in Texas on using community resource and referral platforms to identify and address non-medical drivers of health. While geared to a Texas audience, lessons herein can inform activities in other states to better address non-medical needs of Medicaid populations.
Read Brief -
Resource
Cross-Sector Data Sharing to Address Health-Related Social Needs: Lessons Learned from the Accountable Health Communities Model
Source: CMS
This report discusses the importance of effective data sharing between clinical and community partners and shares lessons learned from the Accountable Health Communities Model.
PDF ↓