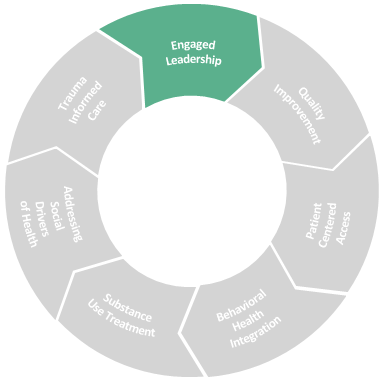
Crucial to sustaining a new model of of team-based care is having leaders who proactively facilitate practice transformation by establishing and communicating the need for change, and then fully supporting the implementation on multiple levels throughout the health center. Transformational change requires that everyone, including leaders, learn new ways of working together to support the individuals and communities they serve.
Drivers of Success:
- Transformational change framework
- Infrastructure and resources to support the Integrated Primary Care Model
- Equity at all levels
Key Resources:
We consider the resources below to be key foundational resources for leading transformational change in healthcare.
-
Resource
NACHC Value Transformation Framework Assessment Portal
Source: NACHC
This portal offers free, online tools designed to guide health centers in areas of system change fundamental to advancing on the Quintuple Aim using NACHC’s Value Transformation Framework.
Visit website -
Resource
The Center for Accelerating Care Transformation
Source: ACT Center
The ACT Center is centered in improving health for people and communities by creating a path from research to practice
Visit website -
Resource
Engaged Leadership Implementation Guide
Source: Safety Net Medical Home Initiative
Learn how to better implement an Engaged Leadership team, along with why it is important and the benefits of doing so.
PDF ↓ -
Resource
The 10 Building Blocks of High-Performing Primary Care
Source: Annals of Family Medicine
The 10 Building Blocks represent the innovative thinking that is transforming healthcare in the United States
PDF ↓ -
Resource
AMA STEPS Forward: Change Initiatives
Source: American Medical Association
Learn how to create an effective change method and produce sustainable improvements within a healthcare practice
Visit website -
Resource
AMA STEPS Forward: Leadership & Culture
Source: American Medical Association
Learn how to successfully lead change and empower a healthcare team to cultivate a supportive and honest culture
Visit website -
Resource
AMA STEPS Forward: Mini Z Burnout Survey
Source: American Medical Association
This survey by the American Medical Association monitors the burnout level of employees in healthcare.
DOCX ↓
Engaged leadership in action
Throughout the toolkit, we will call out specific examples of engaged leadership that are instrumental for success within the individual domains of the IPC Model.
Transformational Change Framework
Creating and modeling the conditions for transformation
There are a multitude of books written about leadership and managing change. The goal of the IPC Toolkit is to highlight the components of leading change that are most aligned with the transformational change attributes and activities that health center leaders must do to successfully implement new models of care. Similar to the adoption of the patient-centered medical home model (PCMH), the implementation of the Integrated Primary Care model requires leaders to:
- Establish the evidence base and need for change, and the vision for the future
- Communicate clearly, often, and in multiple ways the need for transforming how care teams function and the vision for the future model of care, ensuring total alignment of that vision through all levels of the organization and with the communities served
- Commit to all components of the IPC model with an understanding of how each department in the Health Center is affected by the transition of roles, workflows, compensation, etc.
- Periodically measure health center’s team-based care model using a value-based care self-assessment tool and staff satisfaction, identifying strengths and opportunities for improvement efforts
- Acknowledge that transformational work takes time and perseverance; appreciate and reward everyone’s participation in the endeavor
A leadership framework that may be a useful, practical guide to transformational change is Kotter’s The 8 Steps to Leading Change.
| 1. Create a sense of urgency | Inspire people to act – with passion and purpose – to achieve a bold, aspirational opportunity. Build momentum that excites people to pursue a compelling (and clear) vision of the future… together. |
| 2. Build a guiding coalition | A volunteer network needs a coalition of committed people – born of its own ranks – to guide it, coordinate it, and communicate its activities. |
| 3. Form a strategic vision | Clarify how the future will be different from the past and get buy-in for how you can make that future a reality through initiatives linked directly to the vision. |
| 4. Enlist a volunteer army | Large-scale change can only occur when massive numbers of people rally around a common opportunity. At an individual level, they must want to actively contribute. Collectively, they must be unified in the pursuit of achieving the goal together. |
| 5. Enable action by removing barriers | Remove the obstacles that slow things down or create roadblocks to progress. Clear the way for people to innovate, work more nimbly across silos, and generate impact quickly. |
| 6. Generate short-term wins | Wins are the molecules of results. They must be recognized, collected, and communicated – early and often – to track progress and energize volunteers to persist. |
| 7. Sustain acceleration | “The way that you can guarantee success in a difficult change… is to not skip any of the steps or the learnings.” |
| 8. Institute Change | Articulate the connections between new behaviors and organizational success, making sure they continue until they become strong enough to replace old habits. Evaluate systems and processes to ensure management practices reinforce the new behaviors, mindsets, and ways of working you invested in. |
-
Resource
Kotter’s The 8 Steps to Leading Change
Source: Kotter
Kotter showcases its developed methodology of common success factors that lead to making a change
Visit website -
Partner Resource
Designing our Future Blog
Source: Lynn Community Health Center
The former CEO of the Lynn Community Health Center documented & shared their health center’s journey to value-based care in this series of blog posts.
Visit website
Health Center Infrastructure to Support IPC
The transition away from fee-for-service to value-based care requires that health center leaders intentionally invest in creating the environment and systems to support transformation.
This is the “how-to” for creating the culture of innovation. It requires using and analyzing data, empowering care team champions, redefining care team roles, integrating new members to the team, and optimizing technology, workflows, and systems to support and sustain the new way of delivering care to patients.
Concrete components include:
- Consider creating one or more Practice Transformation Team (PTT) that includes a representative from all care team roles, e.g., a provider champion, medical assistant, nurse, community health worker, social worker, recovery coach, care coordinator, and/or other care team role. Leadership must create the opportunities for the PTT to meet, establish trust and norms of collaboration, and carry out tests of change in the health center. This includes communication and buy-in throughout the health center so that staff who may need to cover for a colleague who is working on a test-of-change knows his/her/their role is as critical as their colleagues’. The PTT team must be fully understood and supported by the entire organization.
- Develop and cultivate one or more Provider Champion to serve and help lead the work of the PTT(s) and to engage all the providers in the health center.
- The PTT and leaders who are advancing change must use measurement and a data-driven approach to the work. See the Quality Improvement section for information and resources on data driven approaches.
- Optimizing the Electronic Health Record (EHR) and creating workflows that are clear and documented to support care teams in carrying out the new ways of working together is critical. Consider creating a Care Team Toolkit or Manual specific to your health center that defines the roles of the team and the tools they use to carry out required tasks and function. Utilize the front line to inform the creation of the manual and create processes to keep it fresh and updated.
- Engage in a process to develop a new Compensation Model for providers and teams. This includes developing a new philosophy around compensation, communication throughout the health center, and using new measures related to patient outcomes and quality results. It requires a deliberate move away from productivity as an incentive and gaining buy-in across the organization, including finance and operations leaders and managers.
- Invest in Staff Wellness / Preventing burnout. Develop a culture of ‘staff-centeredness’ where the health and wellbeing of staff is surveyed, and results are shared and acted upon. See the Trauma-informed Care section for more information and resources.
- Part of investing in Staff Wellness includes providing Ongoing Training and Professional Development opportunities for staff. Consider reserving time for care teams to engage in ongoing training during work hours by creating systems for rotation and coverage and/or by blocking schedules periodically for this important investment in staff.
- Including Human Resources (HR) is essential to the creation of new roles, care team integration and ongoing professional development needs. Often HR is brought in at the end of the process. Partnering with HR earlier in the transformation journey facilitates organization-wide buy-in and embeds the transformation work more deeply in the processes of recruitment, hiring, retention and training.
-
Resource
Practice Improvement Team Toolkit
Source: Cambridge Health Alliance
Learn from Cambridge Health Alliance about the work of a Practice Improvement Team and the benefits of having one in a healthcare setting
PDF ↓
Equity at All Levels
Achieving equity within a health center and striving for health equity outcomes in the communities served by health centers are broad, complex goals. For the purposes of this toolkit, the focus is on the fundamental approaches that leaders must do to promote equity. Additional resources are included within other sections of the toolkit, including Social Drivers of Health and Quality Improvement.
Approaches to achieve equity within health center Care Teams:
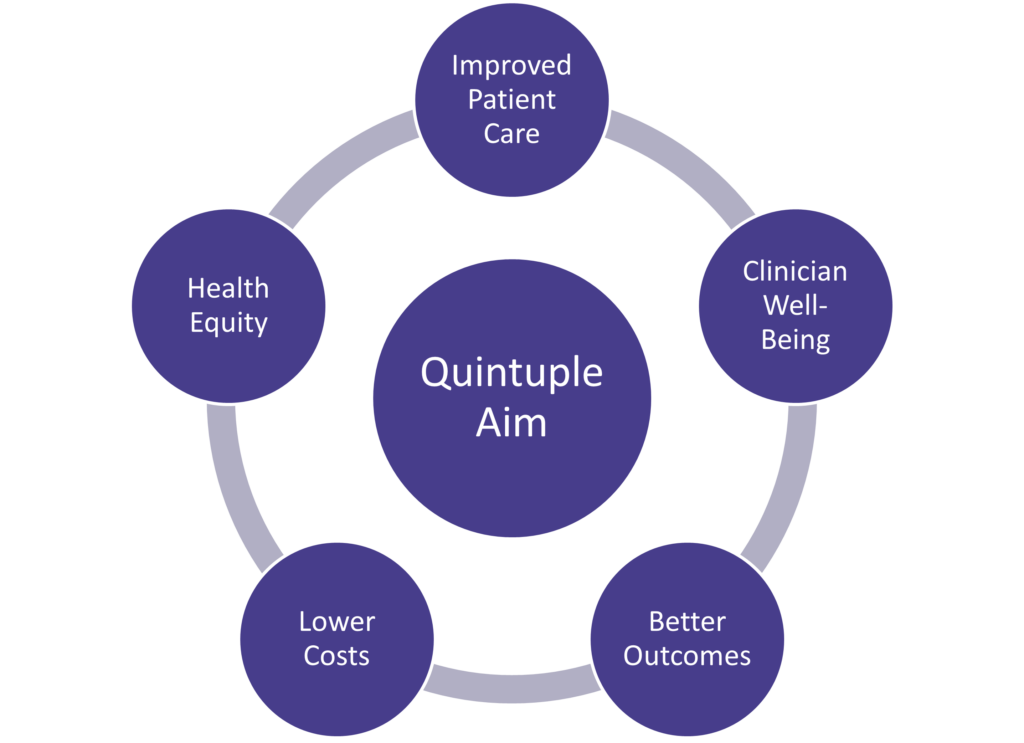
- Strategy: Leaders should ensure that equity is clearly communicated to all as a core part of the health center’s Annual Plan and overall strategy so that Care Team members understand their roles in the bigger picture of their organization. The IHI Quintuple Aim of improving population health, enhancing the care experience, reducing costs, and achieving health equity may be a useful approach to share, especially as a visual tool:
- People: The partnership between leaders and Human Resources is critical for hiring diverse staff and for fostering a work culture of inclusion and belonging. Additionally, attention should be paid to hiring from the communities served and for alignment of staff and providers’ linguistic capabilities with the patient population.
- Innovation: Foster opportunities for all Care Team members to meaningfully participate in quality improvement and innovation activities. Methods to engage staff in efforts to achieve the objectives of the Quintuple Aim include – inviting staff to join a quality improvement or practice transformation committee, conducting staff focus groups on how to improve team based care, shadowing staff in their day-to-day roles to learn how their workflows support patient care. The more that all Care Team members are included in these efforts, the more comfortable staff are in voicing novel or “out of the box” ideas to streamline and/or improve working with others and serving their patients.
- Patient Partnership: Traditionally, patients and their families are encouraged to be deeply engaged in their own care. To promote more equitable workflows that center the patients on the Care Teams, health centers may go beyond the traditional approach and develop standing and/or Ad Hoc Patient Partner positions. Patient Partners are those seeking care at the health center who have the bandwidth and interest to participate in activities to improve Care Team workflows. Cambridge Health Alliance has a chapter in their Practice Improvement Team guide on how to accomplish this work, which can be high effort but achieves high reward in regards to equity.
-
Resource
Practice Improvement Team Toolkit
Source: Cambridge Health Alliance
Learn from Cambridge Health Alliance about the work of a Practice Improvement Team and the benefits of having one in a healthcare setting
PDF ↓ -
Resource
Building Toward Racial Justice and Equity in Health: A Call to Action
Source: Massachusetts Attorney General’s Office (AGO)
This report discusses ways stakeholders should come together to address the systemic health inequities facing people of color.
PDF ↓
-
Resource
On the Quintuple Aim: Why Expand Beyond the Triple Aim?
Source: IHI
This blog post discusses expanding the original Triple Aim (improving population health, enhancing the care experience, reducing costs) beyond the “quadruple aim” (addressing clinician burnout) to a “quintuple aim” that includes advancing health equity.
Visit website -
Resource
The Quintuple Aim for Health Care Improvement: A New Imperative to Advance Health Equity
Source: JAMA
This article proposes expanding the original Triple Aim (improving population health, enhancing the care experience, reducing costs) beyond the “quadruple aim” (addressing clinician burnout) to a “quintuple aim” that includes advancing health equity.
Visit website
Approaches to advance health equity in the communities served:
- Expanded Care Teams: Incorporating positions including Community Health Workers, Recovery Coaches, and Family Partners on Care Teams creates an environment where more staff to share the care of patients. This approach allows for a patient to closely work with someone in addition to or other than their Primary Care Provider, which promotes a trauma-informed culture for patients who may historically not trusted medical providers.
- Data Driven Approach: Leaders who resource and support robust data analytics are able to employ data driven approach to understanding health inequities (across all domains) that exist within their patient population.
- Telehealth: Leaders who embrace telehealth offer their patients more choices in how to get their care in a safe and timely manner. The inclusion of screening for digital access within health related health needs screening creates opportunities for patients to receive referrals and education on devices, broadband, and digital literacy.
- Social Health: Leaders must prioritize partnerships with community based social service organizations and public partners in order to achieve improvement in the social health of their communities. While Care Teams are responsible for screening for and addressing health related social needs, these staff and providers are limited in their impact without meaningful leadership engagement in the social drivers of health.
-
Resource
Achieving Health Equity
Source: Robert Wood Johnson Foundation
A comprehensive set of resources from the RWJF
Visit website