Value-Based Care
Health Centers are the foundation of health care for low-income, under-resourced populations in the United States. They provide high quality care and lower total cost of care than other primary care settings (APHA, 2016). Like many providers, however, health centers rely on per visit, fee-for-service (FFS) payment for much of their revenue. In this payment model, only visits with licensed clinicians are reimbursed and many short visits per day are required to generate sufficient revenue to support the cost of health center operations. Many activities now viewed as essential in caring for the health of a population are not reimbursed, such as a telephone call from a community health worker, a home visit by a nurse, or a care team meeting. Health centers have the potential to deliver even better care and lower total costs for populations if they can overcome the limitations of the FFS system (Harvard Business Review, 2020).
The market trend known as “value-based care” seeks to overcome payment impediments to population health by paying per person for health care and health outcomes rather than per visit (Harvard Business Review, 2016). In 2017, 34% of U.S. health care payments were made in some type of value-based care arrangements. Nationally, Medicaid lags behind other payers in the movement to value-based care; payment and delivery system innovation is disproportionately centered in for-profit health care delivery organizations (Mckinsey, 2018). We believe low-income and under-resourced populations in the United States should benefit from the same level of disruptive innovation as middle and high-income populations. Although health centers must innovate if they are to continue to serve their mission in an environment of changing health care delivery and payment, ironically the day-to-day trappings of the FFS system put their ability to finance needed change just out of reach.
How to Use This Toolkit
Like the value-based care environment, this toolkit is continuously evolving. New content will be added on an ongoing basis, and updates will be featured here.
This toolkit is intended to be used by anyone involved in leading change within primary care settings, with a particular focus on community health centers. You do not need to read the toolkit in its entirety from start to finish, but we do encourage you to familiarize yourself with the background information found in the Introduction, where we describe our journey to develop the Integrated Primary Care Model and our vision for the Integrated Primary Care Team.
Each section focuses on a particular domain of the Integrated Primary Care Model. Within each section, you will find the key drivers for success in that domain. These drivers were developed through interviews with subject matter experts, a review of foundational models and resources, and our own experience leading practice transformation efforts. Common themes will be found within each section: engaged leadership in action, key care team members, and health equity.
Each section includes a curated collection of resources to support success in that domain. Resources consist of a mix of concrete tools that can be adapted for your health center (job descriptions, etc.), evidence and examples of the work in action (case studies, webinars, literature), and links to our go-to online resources. Partner Resources, which are shown in green boxes, are resources that our developed by C3 and C3’s member health centers.
The Integrated Primary Care Framework

Health centers have worked hard over the last 10-15 years to implement the Patient Centered Medical Home (PCMH) Model of care. As we began to plan for the move to value based care, we asked ourselves what parts of this model need to evolve and what is missing to care for an entire population both inside and outside the walls of the health center. We concluded that the PCMH model lays important groundwork in team-based care and supporting technology. However, in our experience working with our health centers and supporting organizations to achieve PCMH recognition, it is, at best, a baseline for the activities required to be successful with the population health management of complex populations.
One of our first efforts, as we began to conceive of transforming primary care under value-based care was to define what primary care needed to be and do to meet the goals of value-based care. In this context, we developed our Integrated Primary Care model and defined the seven domains that comprise the model, as depicted in the “wheel” image above.
The process to develop the Integrated Primary care model was informed by working with key advisors from our health centers and it was approved by our Quality Committee, composed of health center clinical leadership. For each of the domains depicted, we defined a “domain steward”, the entity that we relied on to define what competence in each area consisted of. In most cases, the steward was a nationally known entity such as SAMHSA or Qualis, Inc.
-
Partner Resource
Advancing Value-Based Care at FQHCs: The Integrated Primary Care Journey
Source: Community Care Cooperative (C3)
This blog post describes C3’s journey to develop the Integrated Primary Care Model
Read blog post
The Integrated Primary Care Team
The other key component of this vision for Integrated Primary Care was designing the primary care team that would deliver it. For this, we did both an initial literature review and consulted with internal and health center experts. Based on this input, we developed a model care team for both adults and for children and adolescents. This model care team is shown below.
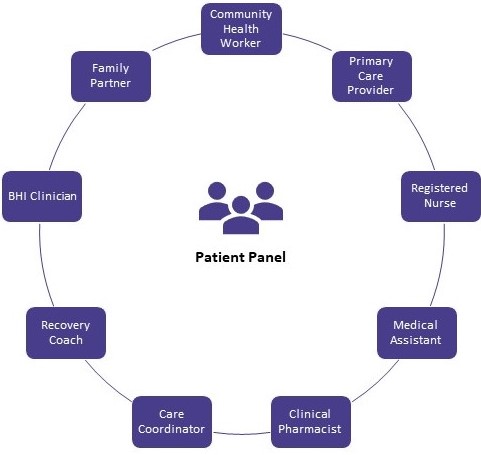
A team-based care approach is necessary for ensuring that patient’s physical, behavioral, and social needs are addressed. As we move away from the FFS payment model and into value-based care models where success is based on health outcomes, it becomes even more important for health centers to design the care team based on the needs of the patients being served. A health center may not have all of these roles, and some functions may be represented by other roles. A value-based care environment allows for more flexibility and innovation in care team roles than a FFS environment. Read more about optimizing patient roles in the Patient-Centered Access section.
Care Team Principles in Value-Based Care
- The patient’s primary relationship is with any team member depending on their needs at that time
- The Primary Care team has adequate time to huddle and meet to build trust, cohesion, and role clarity
- Providers have time to meet with all members of the care team to discuss patient care
- Community Health Workers, Care Coordinators, Medical Assistants, Family Partners, Recovery Coaches, and Peer Workers are valued members of the team
- Teams have the flexibility to see patients in the modality that is best for the patient: in clinic, telehealth, at home, in the community
- Each team members works at the top of their license and scope of practice
Key Team-Based Care Resources
-
Resource
Team-Based Care Implementation Guide and Toolkit
Source: Cambridge Health Alliance
This is a model of workflows for implementing Team-Based care for providers and healthcare staff.
PDF ↓ -
Resource
Primary Care Team Guide
Source: MacColl Center for Health Care Innovation
The Primary Care Team Guide provides step-by-step direction on how to establish these high-functioning teams and implement new functions essential to team-based care. Numerous tools and resources from 31 exemplary practices nationwide are made available to support you.
Visit website
-
Resource
CHAMPS Team-Based Care Resources
Source: CHAMPS: Community Health Association of Mountain/Plains States
This website provides an introduction to team-based care and contains tools, articles, and guides on implementing team-based care practices.
Visit website -
Resource
Team-Based Care Toolkit
Source: American College of Physicians
This toolkit shares best practices and real-life examples of successful team-based clinical care models that include internal medicine physicians working with Nurse Practitioners (NPs) and Physician Assistants (PAs) and other members of the clinical care team.
Visit website
About C3
Community Care Cooperative (C3) is a non-profit ACO formed in 2016 by Federally Qualified Health Centers (FQHCs) for FQHCs to participate in value-based health care. We are a fast-growing company currently composed of 22 FQHCs and one affiliated provider practice in Massachusetts which means we are the largest Medicaid ACO in MA serving well over patients enrolled in Medicaid.
In addition, we have launched two subsidiary companies: one focused on pharmacy and one on technology/EHR implementation and optimization. In addition, C3 has ventured into the Medicare space with at least two Medicare contracts with partners both inside and outside Massachusetts. Our mission remains to leverage the collective strengths of federally qualified health centers to improve the health and wellness of the people we serve.