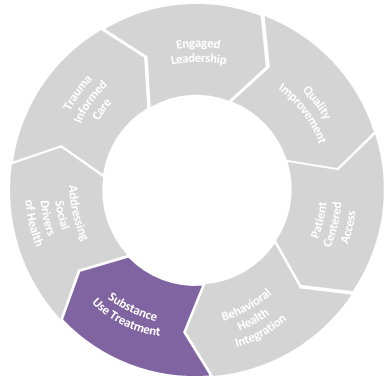
Substance Use Treatment in the IPC Model refers to the full integration of medication for addiction treatment and peer support model, including recovery coaching, in primary care.
Drivers of Success
- Multidisciplinary & team-based approach
- All patients can be screened and treated at all visits by their primary care team
- Engagement with treatment providers in the community
- evidence-based training curriculum for all staff
- The intersection of trauma/BH/SUD/institutional racism is addressed
engaged leaderhsip in action
- Leadership team normalizes conversations about SUD, challenges the stigma often association with SUD, and is visibly supportive
- Provider and staff wellness is prioritized
- All primary care teams are capable of treating all substance use disorders
- Substance use treatment is viewed as a social justice issue
Key Resources:
-
Partner Resource
Best Practices Playbook: Initiation and Engagement of Alcohol, Opioid, or Other Drug Abuse of Dependence Treatment
Source: Community Care Cooperative (C3)
The goal of this playbook is to provide the context, resources, best practices, workflows, and strategies to increase the likelihood that a member will initiate and then engage in ongoing alcohol, opioid, or other drug abuse or dependence treatment.
PDF ↓ -
Resource
Hill Country Community Clinic: Integrating Substance Use Treatment and Support into Primary Care
Source: Center for Health Care Strategies
A profile of one FQHC’s journey to fully integrate SUD services into primary care. Topics covered include adding SUD counselors to primary care teams, training all care team members and staff in addiction-informed care and trauma-informed care, and creating a new complex care coordinator position
PDF ↓
Multidisciplinary & Team-based Approach
Full integration of substance use treatment involves a multidisciplinary, team-based approach. Often, these services are nurse-driven and managed. When substance use treatment is fully integrated into the primary care setting, it can be treated similarly to other chronic medical conditions. Nurses are well equipped to serve as Care Managers. Health centers experience better success when they have dedicated physicians/other prescriber “champions” to support less-experienced clinicians. Non-clinical peers and recovery coaches play a vital role in supporting patients, and it’s important that all members of the care team understand the role of recovery coaches.
A multidisciplinary SUD treatment team includes:
- Registered nurse trained in harm-reduction
- Non-clinical peers & recovery coaches
- Primary Care Providers (MD, DO, NP, PA) for prescribing
- Integrated social worker
- Clinical pharmacists for training/consultation
-
Resource
Peer Support Toolkit
Source: Philadelphia Department of Behavioral Health and Intellectual Disability services
This toolkit is designed to support BH treatment agencies with the process of integrating peer providers into their service setting. However, many tools and recommendations outlined here can also be applied to primary care settings.
View Toolkit -
Resource
Core Competencies for Peer Workers in Behavioral Health Services
Source: SAMHSA
SAMHSA—in conjunction with diverse subject matter experts—conducted research to identify core competencies (the critical knowledge, skills, and abilities needed) for peer workers in behavioral health.
Visit website -
Resource
Nurse Care Manager Model of Office Based Addiction Treatment: Clinical Guidelines
Source: Boston Medical Center
These policies and protocols are meant to provide best practice guidelines to clinicians utilizing buprenorphine and/or naltrexone for the management of opioid use disorders and alcohol use disorders in mainstream medical practices, and to expand access to treatment
PDF ↓
SUD is a complex but treatable disorder and each patient experiences it differently. As a result, care teams may encounter clinical situations where consultation and technical assistance are needed in order to better serve the patient. Organizations like MCSTAP and BMC TTA offer real-time consultation and expert assistance for clinicians on safe prescribing, increasing their capacity for and comfort in substance use treatment.
-
Resource
Massachusetts Consultation Service for the Treatment of Addiction and Pain (MCSTAP)
Source: Massachusetts Consultation Service
MCTSAP supports Massachusetts providers in increasing their capacity for using ways to screen and treat patients with chronic pain and substance use disorders
Visit website -
Resource
Boston Medical Center (BMC) Grayken Center for Addiction Training and Technical Assistance (TTA)
Source: Boston Medical Center
Learn ways to provide education, support and capacity building to community health centers and other healthcare services
Visit website -
Partner Resource
Credentialing Providers to Prescribe Buprenorphine and Developing Integrated Model for the Treatment of Substance Use Disorder
Source: Community Care Cooperative (C3)
This webinar addresses ways in which providers can better support substance use disorders and introduces Buprenorphine as a way to supplement substance use in treatment
Watch webinar
Patients can be screened at all visits and treated at all visits by their primary care team
It’s important that patients can be screened and treated at all of their visits by their primary care team for many reasons:
- Recovery is not linear, and no single treatment is right for everyone
- The more we talk about it, we lessen the stigma and biases
- Early intervention can improve outcomes
The webinar below highlights how one health center uses technology to maintain a Zoom chat room for providers and care team members to facilitate urgent & emergent real time consults. A physician champion, OBAT nurse, and OBAT community health worker monitor the Zoom channel to help get patients in for appointments to start treatment, triage missed visits, refill prescriptions, etc.
-
Partner Resource
Credentialing Providers to Prescribe Buprenorphine and Developing Integrated Model for the Treatment of Substance Use Disorder
Source: Community Care Cooperative (C3)
This webinar addresses ways in which providers can better support substance use disorders and introduces Buprenorphine as a way to supplement substance use in treatment
Watch webinar
Engagement With Treatment Providers in Community
By engaging with treatment providers in the community, you are expanding your menu of options and acting upon the tenet of shared decision-making which puts the patient first.
-
Resource
Massachusetts Community Behavioral Health Centers
Source: Massachusetts EOHHS
Community Behavioral Health Centers (CBHCs) are one-stop shops for a wide range of mental health and substance use treatment programs. The statewide network includes 25 CBHCs in communities across Massachusetts. CBHCs offer immediate care for mental health and substance use needs, both in crisis situations and the day-to-day.
Visit website
Evidence-based Training Curriculum for All Staff
Where you put your time expresses your values and priorities. Beyond complying with federal (DEA) training, leadership should consider giving protected time for staff to assume nonclinical functions such as completing CME courses and trauma-informed care training so that staff are supported in their professional development and continuing education which will also positively impact patient-care team experiences.
-
Resource
AMA list of CME trainings that would fulfill DEA requirement
Source: AMA
The AMA offers a new training requirement issued by the Drug Enforcement Administration for providers to meet the conditions on treating and managing patients with substance use disorders
Visit website -
Resource
National Harm Reduction Technical Assistance Center
Source: CDC
The CDC presents the National Harm Reduction Technical Assistance Center as a resource that provides free help to anyone in the country
Visit website -
Resource
Using Motivational Interviewing in Substance Use Disorder Treatment
Source: SAMHSA
SAMHSA denotes a pamphlet for treating substance use disorder with motivational interviewing
Visit website -
Resource
TIP 42: Substance Use Treatment for Persons with Co-Occurring Disorders
Source: SAMHSA
ThisTIP is intended to provide addiction counselors and other providers, supervisors, and administrators with the latest science in the screening, assessment, diagnosis, and management of co-occurring disorders (CODs).
Visit website -
Resource
Practitioner Training
Source: SAMHSA
SAMHSA organizes a webpage that offers practitioners a list to help navigate the field of substance use and mental health disorders
Visit website
Trauma, Addiction, and Equity
“There is almost nothing you can do in healthcare that is more impactful for equity than treating addiction.”
Dr. Kiame Mahaniah
Integrating addiction treatment into primary care is giving equity to patients. Persons with SUD may face additional HRSN challenges such as increased rates of poverty, homelessness, and digital divide which are often disproportionately experienced by minoritized communities. One study found that Black patients were 70% less likely to receive buprenorphine at their visit than White patients, and another showed 92% of Latinx patients diagnosed with a SUD did not receive addition treatment compared to the concerning national average of 82%(source: https://medicine.yale.edu/news-article/racial-inequities-in-treatments-of-addictive-disorders/). Consequently, health equity should underly and drive all decisions and actions around SUD treatment and its integration into primary care so as not to perpetuate systematic discrimination and other health disparities.
Health Center Initiatives and Innovations:
SUD treatment will look different at one FQHC from another, even when all the drivers of success are implemented. FQHCs have to adapt the framework and integrate service lines into existing, nevertheless unique, staffing and resource parameters for instance. Below are ways FQHCs have expanded and transformed primary care at a cultural and operational level to provide SUD treatment.
- Set X-waiver expectations during hiring. HR can screen for and explain to applicants why an X waiver is required for the job and ask for a notice of intent or training completion. Setting this hiring expectation ensures smooth onboarding and alignment with organizational culture. (link PPT Buprenorphine Tier 3 Support Webinar 1-13-22 FINAL)
- Community Zoom channel for urgent real-time consults. FQHCs can set up a group channel (HIPAA compliant) with care team members for ongoing treatment support. This channel is manned by a physician champion and nurse to facilitate pressing requests. By leveraging tools like telehealth for the prescribing of urgent medication, this solution expands access to patients such as those who cannot make it to their appointment. The benefits extend beyond patient access: the community channel may encourage increased engagement from physicians who are lower volume prescribers as they can use it to seek real-time response and support.