Patient-centered access, also commonly known as enhanced or advanced access, is the practice of implementing and sustaining mechanisms for patients to get the care that they want and need, when they want and need it, and how/where they want and need it.
An accessible health center with no barriers is essential for improving patient outcomes and patient experience of care.
What does an accessible health center look like?
- Patient’s primary relationship is with any team member depending on their needs at that time
- The Care Team has adequate dedicated time to huddle and meet to build trust, cohesion and role clarity and to plan for patient care
- Community health workers, care coordinators, medical assistants, family partners, recovery coaches and peers and other important and similar roles are valued members of the team
- Teams have flexibility to see patients in the modality that is best for the patient: in-clinic, telehealth, at-home, in the community
- Each team member works at their full capacity/licensure
NOTE: This toolkit offers tools and ideas around improving access but does not address workforce availability, geographic proximity of services, or affordability.
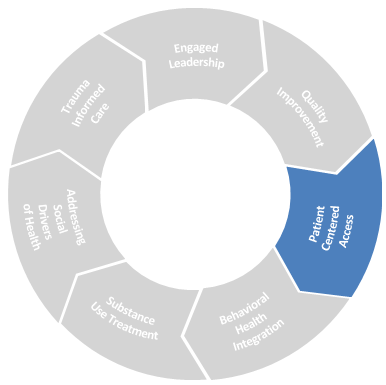
Drivers of Success
- Empanelment
- Management of supply and demand for appointments with PCPs
- Simplification of administrative processes
- Telehealth
-
Resource
Enhanced Access Implementation Guide
Source: Safety Net Medical Home Initiative
This Implementation Guide provides strategies and tactics practices can use to enhance patient access by eliminating barriers to care, balancing supply and demand, and creating capacity to provide care in real-time.
PDF ↓
Empanelment
The Safety Net Medical Home Initiative’s definition of empanelment is “the act of assigning individual patients to individual primary care providers (PCP) and care teams with sensitivity to patient and family preference.” The purpose of this toolkit is to focus on the relationship between a patient and their Care Team, including but not limited to their Primary Care Provider.
Empaneling patients to care teams enables health centers to deliver evidence-based, population health services while striving to achieve balanced patient panel sizes for each care team. Once patients are empaneled, health centers are able to use data and reporting tools to proactively drive improvement in quality of care outcomes and health equity. Additionally, health centers can measure and promote patient continuity of care (visits, phone calls) with their own care team, thereby enhancing the relationships between the patients and their providers.
In an ideal world with adequate care team staffing, panel management requires diligent oversight of panel sizes, patient access data, and patients’ continuity of care with their own care teams. That said, with the reality of understaffed care teams at many health centers, leaders need to go above and beyond to expand patient care to non-traditional members of the care teams (all except primary care providers).
-
Resource
Empanelment: Establishing Patient-Provider Relationships
Source: Safety Net Medical Home Initiative
This implementation guide explains the purpose and process of empanelment and provides step-by-step directions for successful implementation.
PDF ↓
Optimization of Care Team Roles in Patient Care
One of the most ground-breaking aspects of the patient-centered medical home model was the concept of a care team being responsible for the care of a patient, in contrast to the traditional model of the primary care provider/patient dyad. However, with the lack of flexibility care teams have under fee-for-service payment conditions, the ability to innovate with patient care schedule templates has been limited.
Moving forward with team based scheduling in a value based care environment, staff who have not traditionally billed for services are able to take on more responsibilities in the care of a patient panel, promoting workforce satisfaction and growth. Examples of care team encounters with patients outside of the PCP/patient traditional model:
- Diabetes education with Nurse
- Blood pressure re-check with a Medical Assistant
- Follow-up on housing application with Community Health Worker
- Medication reconciliation with Clinical Pharmacist
In one study (see PDF below from the Annals of Family Medicine), a solid portion of a PCP’s workload could be addressed by care team members – including preventative services and chronic disease management. The work of identifying the patients who need PCP-level of care and those whose needs can be met by other care team members is not untenable, but it does require intentional effort and data collection.
-
Resource
Annals of Family Medicine, Patient Panel Size
Source: Annals of Family Medicine
Learn how to better estimate a reasonable patient panel size per primary care physician while having a team-based task delegation
PDF ↓
Care Team Scheduling Under Value-Based Care
The templates below demonstrate one half-day clinical session – under the traditional fee-for-service model and an example of care team scheduling under value based care that breaks away from the traditional model.
-
Partner Resource
Team-Based Care Scheduling Template
Source: Community Care Cooperative (C3)
These templates, adapted from “Effective Team Management,” HMS Center for Primary Care Medical Director Program, demonstrate one half-day clinical session under the tradition FFS system and one under a VBC system
PPTX ↓
It may seem overwhelming to jump from the first template to the second template example. Changing schedule templates requires time and sufficient communication within the health center staff and patients to achieve buy-in and then implement and sustain the innovations. Here are some recommendations for making incremental changes to Care Team templates over time:
Daily Care Team Huddles
- Brief session review conversation at the beginning of each session or each day
- Review patients’ quality of care needs
- Prepare for interpreters, accommodating patients’ special needs for in-person or telehealth appointments
- Review risk coding gaps
- Create plan for reaching out to patients who cancel or do not show for appointments
Weekly Care Team Meetings
- Review patient registries & outreach lists
- Assign follow-up outreach calls and care coordination activities to members of the team
- Coordinate referrals to specialists within and outside of health center; follow-up on important, missed consults and lab tests
- Discuss ideas to improve patient flow within patient care sessions and communication flow outside of patient care sessions
Complex Care Rounds
- Monthly, interdisciplinary meeting to review patients with complex physical, behavioral, and/or social health needs
- Invite Care Managers and others on each patient’s extended care team
- Update patient’s care plan
Longer Appointment Types
- Schedule patients with complex physical, behavioral, and social health needs into longer appointments
- Schedule co-visits with Nurse, Behavioral Health Provider, Pharmacist, or Community Health Worker
- Create time for preventative and chronic disease care
- Coach patients on self-management approaches
Group Visits
- Schedule several patients in one, extended timeslot with a subset of the care team may offer efficiency, improved patient experience, and better clinical outcomes
-
Resource
Group Visit Starter Kit
Source: Group Health
This Group Visit Starter Kit is designed for health care teams who want to begin offering group visits for their patients
DOC ↓
Nurse Visits
- Create standing orders for treatment of common conditions
Panel Management
- Carve-out non-visit time for the care team members to work independently and collaboratively
- Manage eConsults and other referrals
- Population health patient outreach phone calls
- Hospital/ED follow-up
-
Resource
Specialty Care Access in Health Centers – What is the Potential of eConsults?
Source: HITEQ Center
This webinar will discuss innovation in specialty care access using technology and e-Consults. The Maven Project joined the webinar to talk about the particular challenges in specialty care access in health centers and how e-consults can both improve access and support clinicians, including to help to reduce stress and burnout.
Visit website
Simplification of Administrative Processes
Consistent advice across most resources on improving access to care is the suggestion to streamline visit appointment types as much as possible, and by doing so create a straightforward framework for scheduling staff to offer patients appointments that meet the patients’ needs. This approach is grounded in queuing theory.
Another approach for opening-up appointment times for patients in need of synchronous care is to create standardized, reliable non-visit workflows for common requests:
- Prescription refills
- School, camp, work forms
Telehealth
Defining Telehealth – Telehealth is the use of electronic information and telecommunications technologies to support patient care through remote clinical and non-clinical audio and video services, patient and professional health-related training and education, mobile health applications, asynchronous communication via patient portals and text messaging, and home-monitoring/self-care digital communication technologies.
It can be used as a complement to in-person care delivery when clinically appropriate and when a patient has access to broadband, a device such as a phone or computer, and education on how to use telehealth modalities to support their health and wellness.
Optimizing telehealth to improve patient access to care can help to address patients’ barriers to care – including mobility, distance from the health center, and other social health factors. The FQHC Telehealth Consortium has curated a number of resources, including workflows and tools from Massachusetts health centers, into the Telehealth Playbook. The Playbook offers suggestions for how to leverage appointments with Care Team members for the care of patients with chronic conditions. Additional guidance includes promoting patient self-management support, including partnership with nursing staff through the use of remote patient monitoring.
Patient portals are an additional access point for patients and families to interact with Care Team members in an asynchronous manner, avoiding the need for unnecessary appointments – assuming clinical appropriateness.
-
Resource
Telehealth Playbook
Source: Community Care Cooperative
The Telehealth Playbook is a guide that supports the adoption of telehealth in health centers
Visit website