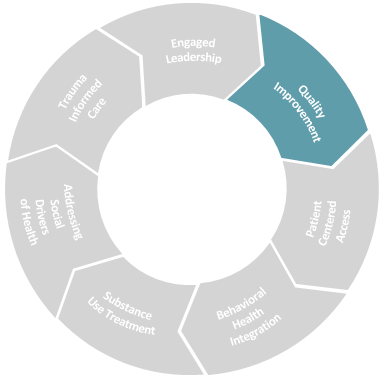
Quality Improvement (QI), as defined by the CDC, includes the “continuous and ongoing effort to achieve measurable improvements in the efficiency, effectiveness, performance, accountability, outcomes, and other indicators of quality to achieve equity and improve health” (Riley, 2010). Because quality of patient care and patients’ experience of care are crucial to value-based care, QI must be pursued and resourced accordingly. According to CMS:
- All Medicare fee-for-service beneficiaries will be in a care relationship with accountability for quality and total cost of care by 2030
- The vast majority of Medicaid beneficiaries will be in a care relationship with accountability for quality and total cost of care by 2030
Many health centers are at different stages in their adoption and utilization of QI, and this toolkit aims to support them in developing QI models and leveraging appropriate tools to be successful in value-based care, regardless of where they are.
QI work requires accountable health center leaders dedicated to performing the core responsibilities from the Safety Net Medical Home Initiative from 2013:
- Understand and articulate to all staff what a fully transformed health center will look like
- Explain how shifting from episode-based care to preventive, comprehensive, empaneled care will help patients achieve optimal health, and will help the practice to function better
- Provide the overall strategy (the What, Why, and How) for QI; Set the vision and provide ongoing support and encouragement
- Describe how staff and patients will fill central roles in the transformation, and how the leaders will support them in this effort
- Provide training and skill set development to enable front-line participation in QI
- Provide visible, ongoing support to QI teams by attending meetings, participating in selected QI activities, reviewing data, and engaging directly with teams
- Understand and articulate how metrics will be used to assess progress
- Monitor progress, provide opportunities to participate, and provide ongoing skill building.
Drivers of Success
- Engagement at all levels of the organization to foster a culture of learning
- Quality structure
- Improvement framework
- Measurement for learning and improvement
Key Resources
There are many excellent resources that provide summary and details information about QI. We consider the resources below to be the key foundational resources.
-
Resource
Quality Improvement Strategy Implementation Guide (part 1)
Source: Safety Net Medical Home Initiative
This implementation guide is designed to help practices select and use appropriate QI methods and measurement tools and how to engage care team members in QI.
PDF ↓ -
Resource
Quality Improvement Strategy Implementation Guide (part 2)
Source: Safety Net Medical Home Initiative
This implementation guide helps practices optimize health information technology to collect, manage, and report data accurately and efficiently.
PDF ↓ -
Resource
Building Quality Improvement Capacity in Primary Care: Supports and Resources
Source: Agency for Healthcare Research & Quality (AHRQ)
This article describes approaches to building improvement capacity in practices.
PDF ↓
-
Resource
Evidence NOW
Source: Agency for Healthcare Research & Quality (AHRQ)
The EvidenceNOW Model for supporting primary care practice improvement originated from a multiyear AHRQ grant initiative designed to advance the adoption of clinical and organizational evidence in small- and medium-sized primary care practices. Click on “Tools for Change” to take a deep dive into tools and resources.
Visit website -
Resource
EvidenceNOW Driver Diagram
Source: Agency for Healthcare Research & Quality (AHRQ)
The EvidenceNOW Key Driver Diagram shows six key drivers—big changes—that primary care practices make to build their capacity to implement the best evidence. For each key driver there are several change strategies—specific actions that support achievement of that key driver. Select any of the key drivers or change strategies to learn more about them. There are tools and resources that correspond to each key driver.
Visit website
Engagement at All Levels
Quality improvement is a scientific approach to testing, studying, implementing, and sustaining practices that improve clinical care and experience of care. When executed effectively, it is an approach that health center leaders can make accessible to staff and care teams throughout the organization, thereby creating norms and behaviors aligned with a culture of learning. To do so, leaders must continuously work at fostering psychological safety so that staff feel comfortable offering novel or “out of the box” suggestions to improve quality. Engagement starts with leadership setting the tone and ensuring that managers and staff have dedicated, protected time for quality improvement activities.
-
Resource
Annual Perspective: Psychological Safety of Healthcare Staff
Source: Agency for Healthcare Research & Quality (AHRQ)
This article describes the important role of psychological safety in healthcare settings and identifies facilitators of and barriers to psychological safety.
Visit website -
Resource
Cultivating psychological safety: Activating humanness in healthcare
Source: Medical Group Management Association
This article describes strategies for cultivating psychological safety and activating humanness in healthcare.
Visit website
-
Resource
A Framework for Safe, Reliable, and Effective Care
Source: IHI
This white paper describes the domains of culture and the learning system, outlining what is involved with each and how they interact; provides definitions and implementation strategies for the nine components (leadership, psychological safety, accountability, teamwork and communication, negotiation, transparency, reliability, improvement and measurement, and continuous learning); and discusses patient and family engagement.
View white paper
Quality Structure
The design and number of leaders and staff in the quality improvement structure of a health center may depend on the size of the population served and the number of services provided. The recommended elements for most health centers includes:
- Clinical Quality Leader
- Quality Manager
- Quality Committee: Leadership team providing quality and risk management oversight, enabling the work of the improvement team
- Practice Transformation Team: Interdisciplinary team with representatives from clinical, operational, and information technology and analytics departments with dedicated time for meetings and improvement/transformation activities
- Annual Quality Improvement Workplan
When possible, the engagement of Patient/Family Partners ensures that the consumers’ voices are heard in identifying opportunities for improvement and developing interventions to address those opportunities. Patient/Family Partners can be engaged through standing committees, ad hoc teams, and through focused surveys to collect feedback on quality improvement interventions being tested by the Practice Improvement Team.
-
Resource
Roadmap to Inviting, Engaging, and Including Patient/Family Partners in Quality Improvement and Other Related Initiatives
Source: National Institute for Children’s Health Quality
The roadmap provides a framework for effective engagement and inclusion of a Patient/Family Partner (PFP) onto a work group, advisory council, Quality Improvement (QI) team, or other clinical or health systems initiatives.
Visit website -
Resource
Practice Improvement Team Toolkit
Source: Cambridge Health Alliance
Learn from Cambridge Health Alliance about the work of a Practice Improvement Team and the benefits of having one in a healthcare setting
PDF ↓ -
Resource
Patient-Center Interactions Implementation Guide
Source: Safety Net Medical Home Initiative
This implementation guide outlines strategies for practice to engage patients in health and healthcare.
PDF ↓
Improvement Framework
A key driver of success in improvement work is the wide-spread adoption of an improvement framework, or methodology. The choice of framework is important, but even more critical is the depth and breadth of the implementation so that all leaders, staff, and providers understand the basic elements of the approach. Without a common understanding and language for identifying and addressing improvement opportunities, quality leaders risk having sole responsibility for improvement initiatives – thereby lessening the success and sustainability of the work.
Two common frameworks are the Model for Improvement and Lean:
- The Model for Improvement includes identifying key questions (What is the aim, What changes will be tested, What will be measured) and plan-do-study-act (PDSA) cycles for continuous improvement.
- Lean uses similar tactics and also emphasizes analyses of processes to identify and eliminate waste in the health center and tasks that do not add value for patients.
-
Resource
Implementation of Lean in a Community Health Center
Source: American Institute for Research
This case study is a snapshot of the overall lean implementation at a community health center during the early implementation period, based on staff interviews, employee surveys, and data on key metrics.
PDF ↓ -
Partner Resource
Using lean thinking to improve hypertension in a community health centre: a quality improvement report
Source: BMJ Open Quality
The objective of this article is to demonstrate system-level improvement in hypertension control in a large FQHC through the situational use of lean thinking and statistical process control.
Visit website
Whether a health center has adopted the Model for Improvement or Lean, the resources below offer easy-to-use tools for Practice Transformation teams and care teams.
-
Resource
Guide to Process Mapping and Redesign
Source: American Medical Association
Process mapping is a simple Lean tool to help you and your team identify inefficient workflows or unnecessary variables in your daily work to head off disorganized and potentially disastrous situations before they arise. This guide describes six steps for process mapping.
DOCX ↓ -
Resource
PDSA Worksheet & Resources
Source: IHI
The Plan-Do-Study-Act (PDSA) Worksheet is a useful tool for documenting a test of change. The PDSA cycle is shorthand for testing a change by developing a plan to test the change (Plan), carrying out the test (Do), observing and learning from the consequences (Study), and determining what modifications should be made to the test (Act).
Visit website
Measurement for Learning and Improvement
Health center leaders are accustomed to assessing data (timely or not) on cost and utilization of services, and quality of care. Engaging all team members in quality improvement work requires all staff and providers to have basic understanding of measurement – where the data comes from, what patients are included, what timeframe, etc. Some common definitions for understanding data from IHI:
Outcome Measures
How does the system impact the values of patients, their health and wellbeing? What are the impacts on other stakeholders such as payers, employees, or the community?
- For diabetes: Average hemoglobin A1c level for population of patients with diabetes
- For access: Number of days to 3rd next available appointment
Process Measures
Are the parts/steps in the system performing as planned? Are we on track in our efforts to improve the system?
- For diabetes: Percentage of patients whose hemoglobin A1c level was measured twice in the past year
- For access: Average daily clinician hours available for appointments
Balancing Measures (looking at a system from different directions or dimensions)
Are changes designed to improve one part of the system causing new problems in other parts of the system?
- For reducing unnecessary home health utilization: Make sure admission rates are not increasing
Data, in the form of score cards or dashboards, may be most utilized by health center leaders and the Board of Directors. To bring measurement to care teams, quality leaders can transparently share progress or updates on process and outcomes measures through staff meetings, health center newsletters, and bulletin boards.
-
Resource
Obtaining and Using Data in Practice: A Handbook for Health IT Advisors and Practice Facilitators
Source: Agency for Healthcare Research & Quality (AHRQ)
This handbook provides the in-depth information Health Information Technology (IT) Advisors need to effectively provide health IT-related assistance for primary care practices to support their quality improvement (QI) and practice transformation efforts.
Visit website