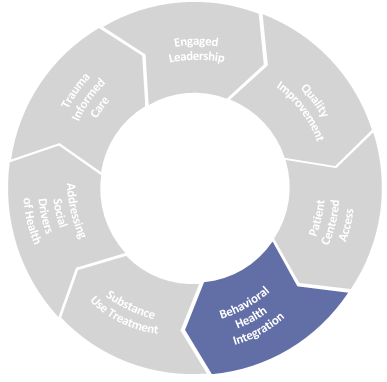
Behavioral Health Integration (BHI) in the IPC model is defined by the full integration of the behavioral health and primary care teams, technology, and processes so that it is one seamless system for patients and families.
Health Centers have long prioritized behavioral health (mental health and substance use) and many have formalized their policies and procedures with the NCQA Patient Centered Medical Home program’s Distinction in Behavioral Health Integration.
-
Resource
NCQA Patient Centered Medical Home program’s Distinction in Behavioral Health Integration
Source: NCQA
Distinction in Behavioral Health Integration helps primary care practices better integrate using Behavioral Health
Visit website
Success of integration of any services at a health center – primary care, behavioral health, specialties such as oral health – requires leadership and collaboration equally from the service lines, as well as ongoing, thoughtful maintenance and improvement of data collection, use of physical space, workflows, and roles. Additionally, the sustainability of integration relies heavily on understanding and maximizing billable services, while expanding non-billable services that are covered under value-based payments and that affect performance in quality of care, patient experience, and total cost of care.
Drivers of Success
- Integration of services framework
- Optimization of care team roles
- Seamless care coordination
- Community engagement
Key Resources
There are many excellent resources that provide summary and details information about BHI. We consider the resources below to be the key foundational resources for BHI.
-
Resource
The National Council for Mental Wellbeing
The National Council for Mental Wellbeing is a webpage that outlines various resources for people to use to help support them when needed
Visit website -
Resource
Comprehensive Integration Framework
Source: The National Council for Mental Wellbeing
A framework for guiding implementation of integrated physical health and behavioral health to help you measure progress in organizing delivery of integrated services,
PDF ↓ -
Resource
Comprehensive Integration Framework Levels
Source: The National Council on Mental Wellbeing
This pamphlet outlines a Behavioral Health integration framework plan
PDF ↓ -
Resource
Agency for Healthcare Research & Quality, AHRQ Academy: Integrating Behavioral Health & Primary Care Playbook
The AHRQ Academy developed the Playbook as a guide to integrating behavioral health in primary care and other ambulatory care settings to help improve health care delivery to achieve better patient health outcomes
Visit website -
Resource
Scaling Behavioral Health Integration in Primary Care
Source: NEHI (Network for Excellence in Health Innovation)
This report offers insights on expanding the integration of behavioral health in primary care settings to improve access
PDF ↓ -
Resource
What are Patient Preferences for Integrated Behavioral Health in Primary Care?
Source: Journal of Primary Care & Community Health
This article shares findings from a research project to determine patient preferences for integrated behavioral health within primary care.
Visit website -
Resource
The Primary Care Behavioral Health (PCBH) Model
Source: Journal of Clinical Psychology in Medical Settings
This article provides a concise, operationalized definition of the PCBH model.
Visit website -
Resource
Primary and Behavioral Health Care Integration Program: Impacts on Health Care Utilization, Cost, and Quality
Source: US Department of Health and Human Services
This reports presents results of analyses of the impact of the Primary and Behavioral Health Care Integration grant program on utilization, costs, and quality of care
PDF ↓ -
Resource
Behavioral Health Integration Compendium
Source: AMA
This compendium is a tool for physicians and their practices to learn about and implement behavioral health integration.
PDF ↓
Integration of Services Framework
Whether a health center is launching a new integration of service lines or is exploring ways to improve an existing BHI program, one important early step is to assess the current state of leadership engagement, workforce, and other capacity concerns through an assessment tool.
-
Resource
NACHC Assessment tool
The Value Transformation Framework is a model that guides an institution’s change by creating actionable steps for the organization to take
Visit website -
Resource
AHRQ Assessment Checklist
Source: Use this self assessment to learn where your organization stands with respect to all aspects of integrating Behavioral Health and Ambulatory Care
Visit website
A comprehensive integration framework includes workflows for screening, brief interventions, population health management, and specialty referrals. Key information for leaders developing a BHI program is to understand the health center population’s behavioral health needs. Helpful considerations include:
- What are the most prevalent diagnoses in our population that can best be addressed in the primary care setting?
- What are the available community resources to refer patients for serious mental illness or conditions that require specialty care?
- Will children, adolescents, and adults all benefit from integration? Which population-based or diagnosis-based approaches will be implemented first and which ones addressed over time?
-
Resource
Advancing Integrated Mental Health Solutions
Source: AIMS Center
An FQHC interested in implementing a program that focuses on addressing depression and anxiety in adults may want to select an integration framework based on the AIMS Center’s Collaborative Care model.
Visit website -
Resource
TEAMUP for Children
The TEAMUP for Children’s Transformation Model is a health center-based model for pediatrics and adolescent medicine
Visit website -
Resource
Telehealth Playbook: Behavioral Health Integrated Pathways
For additional resources on how to successfully integrate telehealth please visit our Telehealth Playbook section on BHI.
Visit website
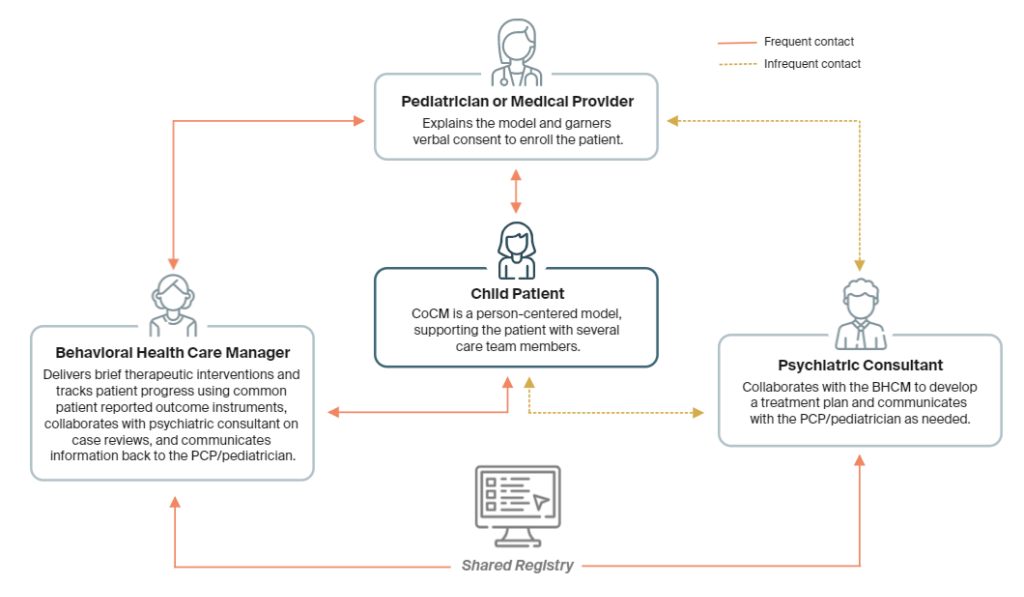
Optimization of Care Team Roles
A fully integrated primary care behavioral health team includes licensed behavioral health clinicians and staff performing care coordination, as well as a consulting psychiatrist. Clinician staff may be Licensed Social Workers or Psychologists and are best suited to receive “warm hand-offs” of patients based on positive screenings or clinical indications identified by primary care clinicians while the patients are being seen in-person or virtually. BH clinicians may also receive referrals to do brief, time limited interventions.
Example of General Workflow for BHI in Primary Care Visits
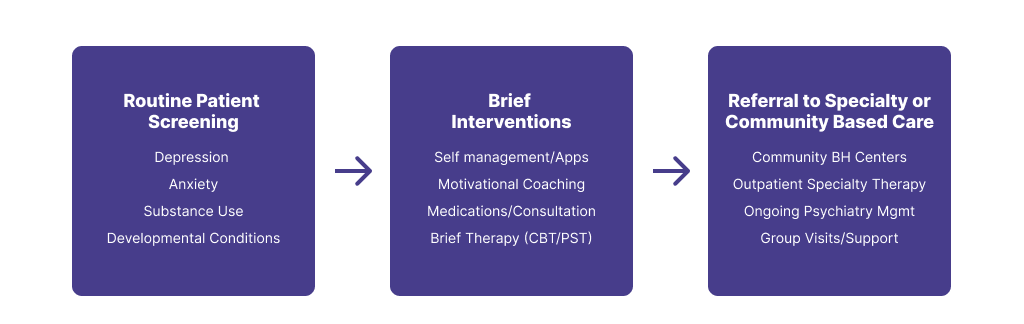
Staff who do not have clinical licenses are critically important in population health management and care coordination of patients and families with identified needs. This work can be done by roles with titles such as Care Partner, Family Partner, BH Coordinator, etc. These staff may also be trained in working directly with patients and families on self-management support tools such as sleep hygiene, mindfulness, and using technology-based health tools. Vinfen has researched and identified many smartphone apps for self-management of behavioral health concerns.
-
Resource
Care Partner Job Description
Source: Cambridge Health Alliance
This is an example of a job description that a health center may publicize to add to the healthcare workflow environment
DOCX ↓ -
Resource
Family Care Partner Job Description
Source: Cambridge Health Alliance
This is an example of a job description that a health center may publicize to add to the healthcare workflow environment
DOCX ↓ -
Resource
Vinfen App Library
A curated list of smartphone apps for self-management of behavioral health concerns
Visit website
Collaborative Care Model Team Member Interactions
-
Resource
How Changes in Medicaid Can Help Primary Care Providers Treat Patients with Behavioral Health Conditions
Source: The Commonwealth Fund
A blog post from The Commonwealth Fund discusses how primary care providers can play a crucial role in behavioral health care, especially when working in consultation with behavioral health specialists.
Read Article
Seamless care coordination
What makes integrated care more effective than co-located primary care and behavioral health services is the partnership, blending of cultures, and shared tools. An integrated care team utilizes the same physical space in a health center, a shared electronic health record, and ideally, and shared treatment plan for co-managed patients.
In addition to the above structures that support integrated care, BHI models promote regular team meetings to discuss overall patient care workflows, population health registries, and complex patient care when necessary. Dedicated, protected time for teams to meet is a key facilitator of the integrated model.
The tools that integrated teams use may depend on the capabilities of the electronic health record or population health management system but should at a minimum include:
- Shared care/treatment plan template
- Patient registries for population health management for conditions/issues requiring close follow-up (depression, early intervention for children)
- Alerts for patients who are admitted or discharged from hospital settings